Estimating the influence of stroke lesions on MEG source reconstruction
Abstract
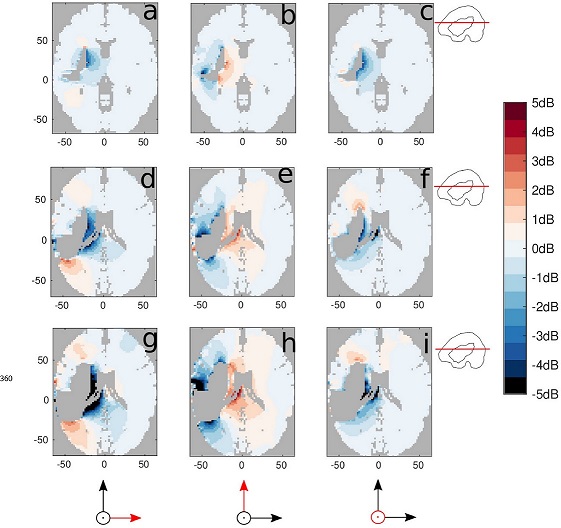
Source reconstruction of magnetoencephalography (MEG) has been used to assess brain reorganization after brain damage, such as stroke. Lesions result in parts of the brain having an electrical conductivity that differs from the normal values. The effect this has on the forward solutions (i.e., the propagation of electric currents and magnetic fields generated by cortical activity) is well predictable. However, their influence on source localization results is not well characterized and understood. This is specifically a concern for patient studies with asymmetric (i.e., within one hemisphere) lesions focusing on asymmetric and lateralized brain activity, such as language. In particular, it is good practice to consider the level of geometrical detail that is necessary to compute and interpret reliable source reconstruction results. To understand the effect of lesions on source estimates and propose recommendations to researchers working with clinical data, in this study we consider the trade off between improved accuracy and the additional effort to compute more realistic head models, with the aim to answer the question whether the additional effort is worth it. We simulated and analyzed the effects of a stroke lesion (i.e., an asymmetrically distributed CSF-filled cavity) in the head model with three different sizes and locations when performing MEG source reconstruction using a finite element method (FEM). We compared the effect of the lesion with a homogeneous head model that neglects the lesion. We computed displacement and attenuation/amplification maps to quantify the localization errors and signal magnitude modulation. We conclude that brain lesions leading to asymmetrically distributed CSF-filled cavities should be modeled when performing MEG source reconstruction, especially when investigating deep sources or post-stroke hemispheric lateralization of functions. The strongest effects are not only visible in perilesional areas, but can extend up to 20 mm from the lesion. Bigger lesions lead to stronger effects impacting larger areas, independently from the lesion location. Lastly, we conclude that more priority should be given to usability and accessibility of the required computational tools, to allow researchers with less technical expertise to use the improved methods that are available but currently not widely adopted yet.